Cosmetic Non-Surgical Rx Reconstructive Surgical Rx Squamous cell carcinoma Sebaceous cell carcinoma Malignant melanoma Trimalar (tripod) fracture Lacerations |
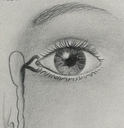
LACRIMAL RECONSTRUCTIONGENERAL CONSIDERATIONS The tear drainage system consists of two small openings called punctum, one in your upper eyelid and the other in the lower eyelid. Each of these openings leads into a small tube called the canaliculus which, in turn, empties into the lacrimal (tear) sac located between the inner corner of your eye and your nose. The lacrimal sac then leads into the nasolacrimal duct that passes through the bony structures surrounding your nose. Tears entering this drainage system empty into your nasal cavity. Functionally, when you blink your eyelids push tears evenly across your eyes to keep them moist and healthy. Blinking also pumps tears into the punctum where the journey through the drainage system begins. If the tear drainage system is blocked at any significant location, your tears back up and spill over your eyelids as if you were crying. Tears that become trapped in the lacrimal sac also can become stagnant with a resultant secondary infection. The most common symptom of lacrimal obstruction is excessive watering/tearing. It can be accompanied by mucous discharge, eye irritation, and painful swelling at the inner corner of your eyelids (the medial canthus). The history and examination usually reveal the location and cause of the obstruction. In office irrigation of your tear drainage system confirms the location of obstruction and determines whether the blockage is partial or complete. This is usually a surgical condition. If a tear drainage obstruction goes untreated, an infection may result - sometimes leading to the formation of an abscess, cellulitis (soft tissue infection), or fistula (an abnormal channel extending from the lacrimal sac to the skin). In the case of abscess or cellulitis, this needs to be treated with topical and systemic antibiotics, along with heat to eradicate the acute infection. Once this is accomplished, surgery is indicated to not only resolve the tearing related to obstruction, but to also prevent a recurrent infection to which you are predisposed. All other cases of lacrimal obstruction require surgery if your tearing symptoms are of a sufficient magnitude to justify this. The location of the obstruction determines the appropriate surgical procedure. SURGICAL TREATMENT If the obstruction is between the lacrimal sac and the nose, a dacryocystorhinostomy (DCR) is indicated. In this procedure the obstruction is surgically bypassed, carrying tears to the nose through the surgically created pathway. This procedure can be carried out either through a skin incision (with a 90-95% success rate) or an intranasal endoscopic approach (with an 85-90% success rate). A fine soft silicone stent (Quickert tube) is placed at surgery for 4 to 6 months - to ensure that the surgical bypass remains open and functional during the postoperative healing phase. If the obstruction is at the canalicular level, a conjunctivo-dacryocystorhinostomy (C-DCR) is indicated. This involves surgical placement of a permanent small Pyrex glass tube (Jones tube) - extending from the inner corner of the eyelids to the nose. These tubes are sized in 1mm increments so that in surgery the proper length tube is placed in conformity with each patient's particular anatomy. These tubes are inert, rarely move, and have a negligible incidence of breakage. Jones tube procedures have a 95% success rate. If you have obstruction in the lower punctum from punctal stenosis (scarring at the punctum with diminution the size of this opening), this is treated via a lower punctoplasty in conjunction with Quickert silicone intubation. The punctoplasty enlarges the pathologically small punctum to approximately 3 times normal size - to allow for permanent entry of tears into the tear drainage system. The Quickert tubes ensure that the enlarged punctum remains open during the healing period to ensure that this structure remains permanently enlarged and functional. All lacrimal procedures are performed under general anesthesia on an outpatient basis. If the obstruction is in a young child, this is the result of an incompletely developed nasolacrimal duct. Up to 7% of children have this problem. In some children the duct will spontaneously open up during the first year of life. If it does not open and symptoms persist, this is treated with lacrimal probing in the operating room. This brief procedure involves passage of a fine metal probe through the patent portions of the lacrimal drainage system (punctum, canaliculus, lacrimal sac) to and through the point of obstruction at the junction of the nasolacrimal duct with the nose - an area called the Valve of Hafner. In severe or recurrent cases, or in children whose treatment has been delayed, the probing is performed in conjunction with Quickert silicone intubation. Treatment of nasolacrimal duct obstruction via probing or Quickert intubation has an extremely high rate of success. All lacrimal procedures are performed under general anesthesia on an outpatient basis. AFTER SURGERY Pain is negligible after surgery and no patch is required. Patients simply use antibiotic ointment at bedtime for 7 - 10 days. If a skin incision was used, sutures are removed 7 to 10 days later in the office. The Quickert tube remains in place as a stent for 4 - 6 months. In most cases it takes 30 seconds to remove the Quickert tube while you are sitting in an examination chair. If the tube has remained in place for its recommended duration, once removed there should be no further tearing symptoms related to tear drainage obstruction. RISKS AND COMPLICATIONS Bleeding and infection, which are potential risks with any surgery, are very uncommon. Minor bruising and swelling may be expected at the surgical site for one to two weeks. Uncommonly, scar tissue may later form, blocking the newly created lacrimal drainage system. Should this develop, surgical revision would subsequently be required.. CONCLUSIONS Lacrimal drainage system surgery has a very high rate of success in bypassing various sites of lacrimal obstruction - thus resolving the associated tearing symptoms. Most patients experience resolution of their tearing and discharge once surgery and stent removal is completed, with little, if any, postoperative discomfort. Tearing Santa Barbara | Tearing Bakersfield |